- Platform
- About us
- Resources
- Events
WhiteSpace Health Blogs
Average Patient Wait Times Increasing for an Appointment, How Long is too Long?
Recently, a new survey by AMN Healthcare was released that detailed the increases in patient wait times before a doctor’s appointment over the last two decades. While this survey only tracked appointments in OB/GYN, cardiology, orthopedic surgery, dermatology and family practice, the results demonstrate the growing impact scheduling is having on patient access to care. Based on this data, it is clear no appointment slots can be wasted if healthcare is to improve patient access, which also drives provider utilization and billings.
Survey Findings
Generally, Wait Times are Increasing.
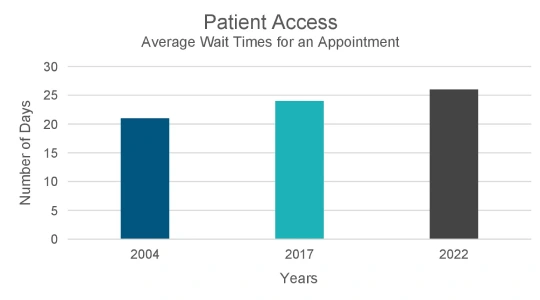
In more than a decade, patient wait times for a doctor’s appointment have increased across five specialties in 15 top US markets. Scheduling a new patient visit with a physician takes 8% longer than it did in 2017 and it takes 24% longer than it did in 2004. While the survey pointed to a growing physician shortage in the US, a constellation of other factors that are likely to be influencing this trend too.
For example, it is unclear whether the acquisition of physician practices by hospitals and health systems and private equity during the pandemic is playing a role. The acquisition of so many practices during the pandemic by private equity and hospitals and health systems that have different scheduling and EMR systems can also add complexity to the scheduling process that is frustrating for the scheduling team as well as patients, causing them to consider seeking alternative care.
Credentialing of providers is another potential source of delay. While providers are in the process of being credentialed, they cannot treat patients. Until providers (MD, DO, PA, NP, etc.) are credentialed at the organization and the location level by various payers, they cannot render services and secure reimbursement.
In addition to administrative barriers and shortages of providers, there are also plenty of articles on healthcare equity that name transportation as a key contributor to patient no-shows and cancellations. Double-booking at-risk appointments and providing complimentary transportation are strategies that are being deployed to mitigate risk.
Family Medicine is the Exception
It's interesting to note that this trend does not apply evenly to all medical specialties. While cardiology and orthopedic surgery appointment wait times have among the highest wait times for a new patient to see a provider, family practice wait times have decreased by 30% since 2004.
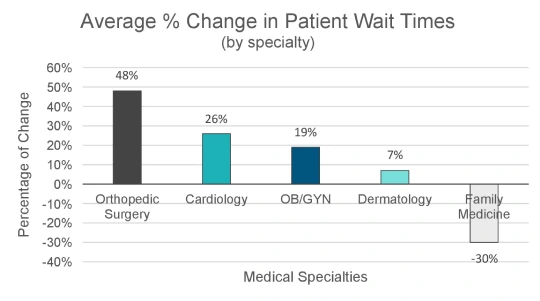
The improved access to family practice care may be attributed to several factors. The consumerism trend that is taking hold in healthcare has resulted in a profound increase in the number of freestanding urgent care clinics. Big box retail pharmacies such as CVS, Wal-Mart and others have also added urgent care product lines to their brick-and-mortar stores. Many of these fully leverage physician extenders for what is normally a lower level of patient acuity. The expansion of telemedicine has augmented in-person care with web and phone-based options. And, virtual care is now an option that closes the transportation gap when the patient has a phone or other device with internet access.
Reasons for No-Shows and Cancellations
A recent MGMA Stat Poll reports that medical practices are experiencing between a 5 – 20% combined no-show and late cancellation rate among multi-specialty practices. If patients do not show up to an appointment slot that was reserved for them, the slot is wasted, and nobody gets to be seen. The need for the patient’s appointment does not go away and the problem of patient access is compounded by a growing number of patients who also want to be seen in addition to the ones who did not keep their appointments.
There are many reasons patients do not show up for their appointments. AI in the WhiteSpace Heath platform has identified over 50 factors with patients not keeping their appointments. As a product management executive for WhiteSpace Health, I have interviewed many people in healthcare and performed a tremendous amount of due diligence to create innovative solutions to these complex problems and my conclusions closely align with the results generated by AI.
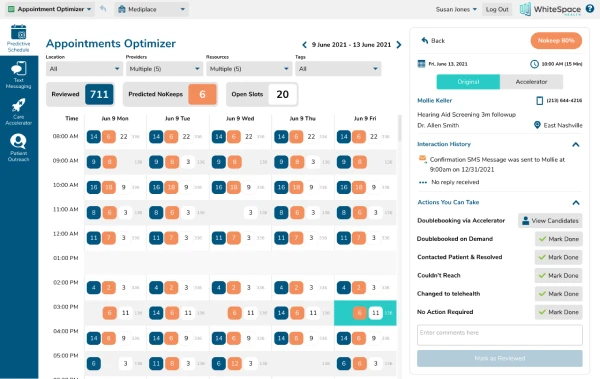
Healthcare Can Adopt Airline Seat Maps for Scheduling
I became interested in applying AI like airlines use to track seat capacity by identifying passengers who are not likely to turn up for their flight. The concept seems to lend itself well to healthcare scheduling. Our Appointment Optimizer product was born from this idea. When used in concert with text-based scheduling, the AI in Appointment Optimizer very accurately predicts which patients are likely to miss their appointments, and your team can double book the slots, mitigating the likely cancellation. This keeps your schedule full, and it ensures timely access to patient care and increased billings.
What are No-Shows and Cancellations Costing You?
From a provider perspective, are you curious how much patient no-shows and cancellations are costing you? Check out my worksheet at the end of this blog post to help you estimate how much patient no-shows and late cancellations are costing.
About Ani Osborne